By Dr Victor Wolemonwu
The overturning of Roe v. Wade in June 2022 by the U.S. Supreme Court, through the Dobbs v. Jackson Women’s Health Organisation decision, fundamentally altered the legal perception of fetal rights in the United States. Before this ruling, the right to an abortion was broadly understood to be an extension of a pregnant woman’s right to privacy and bodily autonomy. This meant that decisions regarding the termination of a pregnancy were primarily left to the individual.
The Dobbs decision, however, eliminated the constitutional right to abortion, returning the authority to regulate or prohibit abortion to individual states. This has led to a significant increase in state-level protections for fetuses, with some states now recognising an unborn child as a person with full constitutional rights. Consequently, in these jurisdictions, terminating a pregnancy not medically necessary for the mother’s health can be considered murder.
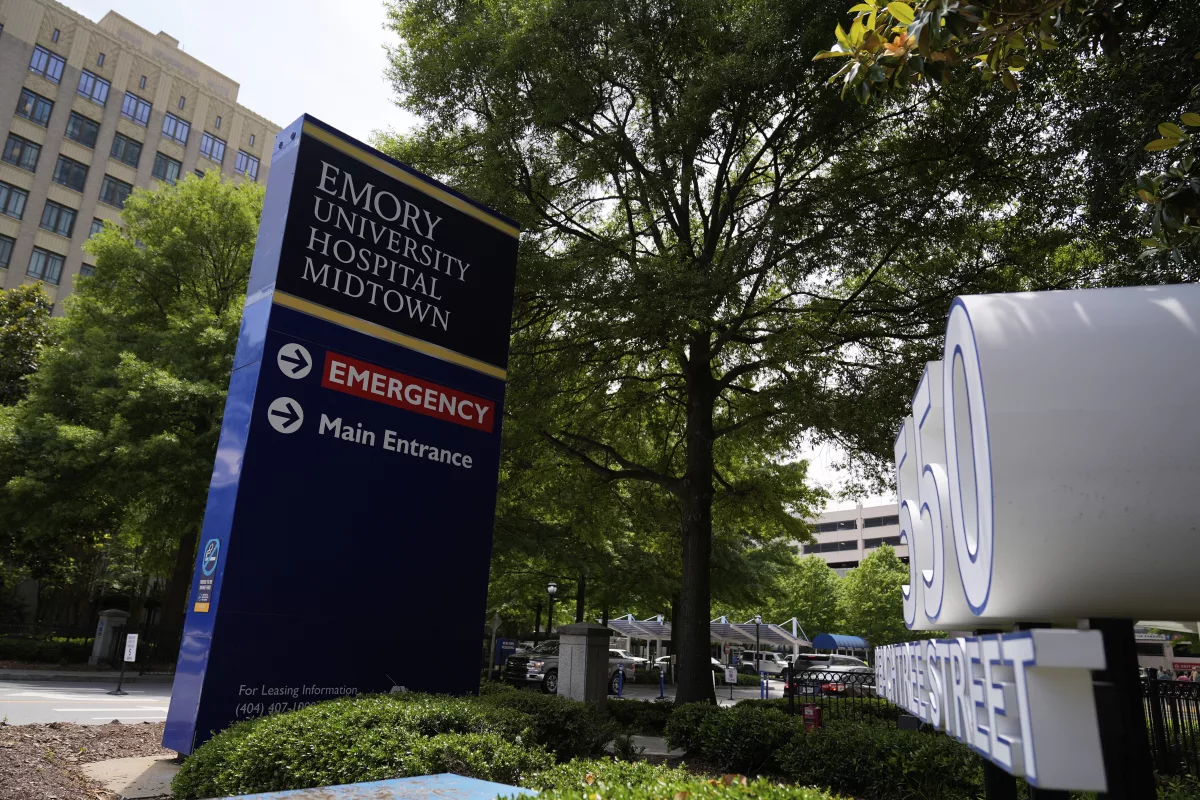
This evolving legal landscape brings forth complex ethical dilemmas, particularly in challenging medical scenarios. A recent case in Georgia involving Adriana Smith, a Black American woman declared brain-dead and subsequently placed on life support to gestate her fetus, exemplifies these complexities. While her mother expressed willingness to care for the child if born alive, she voiced concerns about being excluded from the decision-making process regarding her daughter’s continued life support, questioning whether it was in the best interest of either her daughter or the unborn child.
This case directly intersects with the post-Roe legal environment. If a fetus is legally recognised as a person requiring protection, what are the implications when the pregnant woman is brain-dead? Is it morally permissible for a hospital to maintain life support for gestation when there is no advance directive from the brain-dead woman? Whose best interest should take precedence—the brain-dead woman’s or the fetus’s? Furthermore, what role do family members play in end-of-life decisions for their loved ones in such circumstances?
These are profoundly difficult questions. While many find the prospect of sustaining a brain-dead pregnant woman on life support solely for fetal gestation to be deeply distressing and morally problematic, others argue that such a course of action might not genuinely serve the best interest of the child, given potential complications.
From an ethical standpoint, the hospital’s unilateral decision to maintain life support without consulting the patient’s family raises significant concerns regarding patient autonomy and family involvement in critical medical decisions. The complexity of these issues demands careful consideration of legal precedents, ethical principles, and the profound impact on all parties involved.
What do you think? How can you address the issues raised above?
See the original article for further insights: https://tinyurl.com/mth7akfw